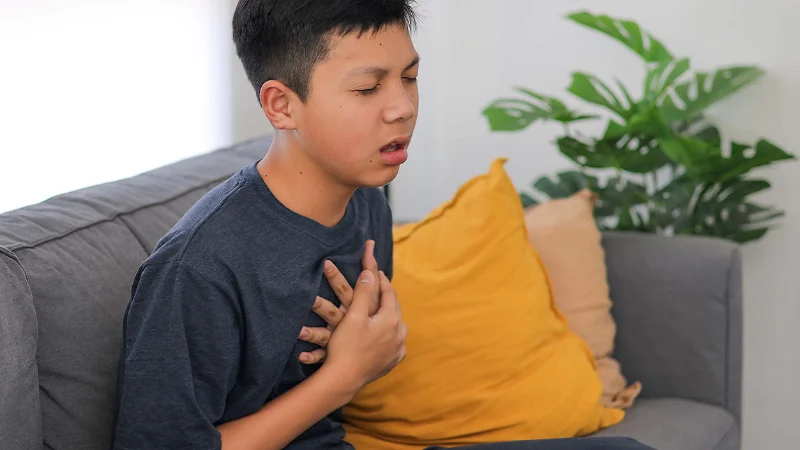
Parents who have children with asthma understand how cold air impacts their condition. However, what is puzzling for parents is why some asthmatic children experience severe winter symptoms yet others with asthma show no signs of severe illness. The answer lies beyond temperature fluctuations.
The development of winter asthma in a child often results from a mix of indoor habits, home setups, and environmental changes which occur in domestic spaces.
Also, some children develop severe asthma flare-ups at specific times during the day including early mornings, after taking bath, and after sleeping under heavy blankets.
Parents will be able to have better know-how for managing winter asthma symptoms and seeking timely care from a pediatrician when they start recognizing these specific patterns.
Why is a Child’s Asthma Worse in Winter? 7 Hidden Triggers Worsening Child Asthma

The main factors which cause winter respiratory problems in children often hide in plain sight. Following are some of the under-discussed triggers that can explain why a child’s asthma is worse in winter.
1. Closed-Room Syndrome in Winter
People usually seal all windows and doors to create a warm environment inside the home. As a result, the room lacks any ventilation or fresh air. The level of indoor CO₂ continues to rise which causes irritation to sensitive airways.
Cooking smoke from the kitchen as well as the particles from incense remain suspended in the air for prolonged periods of time. The surfaces accumulate dust which is inhaled throughout the day.
Thus, the unventilated home environment causes winter asthma flare ups yet most families fail to recognize their sealed homes as the source of their child’s worsening symptoms.
2. Winter Fog + Local Air Pollution Combo
Morning fog isn’t just atmospheric moisture. It traps PM2.5 and PM10 pollutants near the ground level. Children breathe in air in a zone that is lower than adults. The highest levels of pollution exposure occur during school commutes between 7-9 AM.
The toxic particles reach their highest concentration in the air at the most susceptible time, which affects the child’s airways.
Child asthma flare-ups due to pollution in winter is determined heavily by both fog density and traffic patterns, but schools usually do not adjust their outdoor activities based on this information.
3. Heavy Winter Bedding & Seasonal Dust Release
Winter blankets are usually tucked away in storage for eight months when dust mites might have multiplied in the dark space. Taking out these woolen blankets during winter months results in microfiber release which your child breathes during nighttime hours.
Quilts rarely receive sunlight and they are also not put into washing machines. This “winter bedding syndrome” produces winter allergens inside Indian homes that trigger symptoms in children which parents incorrectly identify as cold-weather symptoms.
4. Reduced Sunlight → Vitamin D Drop → Hyperactive Airways
The body produces less vitamin D because of reduced sunlight exposure which leads to hyperactive airway symptoms. In fact, there’s a medical connection between Vitamin D deficiency and bronchial hyperreactivity.
The combination of brief winter days and indoor lifestyle leads to decreased Vitamin D levels in your child. Research shows that children who do not have enough Vitamin D in their system experience more frequent flare-ups.
The airways of these children become extremely sensitive to all triggers including cold air, dust particles, and even laughter. Vitamin D deficiency affects lung tissue responsiveness, and this has less to do with the child’s immunity.
5. Indoor Humidity Inversion
Shutting bathroom doors following hot showers, steam produced by pressure cookers, as well as heat from room heaters leads to moisture buildup that causes mold growth.
The winter humidity pattern produces different conditions than the uniform moisture distribution which occurs during summer months.
Standard advice articles fail to recognize the link between winter humidity and asthma children but mold spores thrive in these specific conditions which cause repeated inflammation.
6. Behavioural Changes in Winter
Your child spends less time outside which leads to weakened lung function because of decreased physical activity. Screen usage rises which leads to developing shallow breathing habits because of extended periods of sitting.
Adding to that, your child might be sleeping under thick blankets which block airflow during the entire night.
This leads to a complicated situation where behavioural changes compound physical vulnerabilities. The winter household habits that trigger asthma go beyond allergens to include behavioural patterns as well.
As a result, it’s important that you keep a watchful eye on how your child breathes, moves, and rests during colder months.
7. Early Morning School Routines
Your child experiences a sudden transition from a hot indoor space to freezing outdoor temperatures at the beginning of their daily commute.
The body constricts the airway passage when it encounters unexpected temperature shifts. The heavy school bag presses against their chest while they take fast breaths in cold air.
The transition from home to vehicle to school during winter mornings creates the perfect conditions for children to develop asthma attacks because their airways experience thermal shock within minutes. That’s why morning asthma attacks in children during winter often occur during this time.
Home heating systems trigger child asthma symptoms because multiple elements work together to create this effect even though parents expect them to help with asthma relief.
The process of heating makes the air dry while it circulates dust particles and reduces the amount of ventilation in the space. This explains why indoor heating worsens child asthma instead of improving it.
Rarely-Debated Symptoms That Parents Miss
Standard advice includes coughing and wheezing as symptoms but no one usually discusses these additional warning signs diagnosed during routine checkups.
Parents often dismiss these as minor discomforts rather than recognizing them as winter asthma symptoms requiring attention:
- Chest pressure specifically during early morning waking
- Sudden post-bath coughing from hot-to-cold temperature shock
- Cough triggered immediately after wearing woolen sweaters
- Silent breathing difficulty during sleep in stuffy rooms
- Rapid breathing visible only upon waking, normalizing later
Asthma in children is worse at night in winter because their room usually lacks sufficient air circulation.
So, if your child has many of these symptoms or the symptoms are persistent, it’s important that you visit the best pediatrician in Gaya at our hospital to get them properly diagnosed and treated. Our pediatrician will work with you to come up with an individualized winter asthma treatment plan for your child.
Top 5 Preventive Steps
The prevention process needs customized preventive actions which replace standard and vague safety protocols. The following methods prove effective in practice:
1. The “Ventilation Hour” Technique
Open all windows in your home for 10-15 minutes during midday when outdoor temperatures reach their highest point. The process removes indoor allergens while it decreases CO₂ levels and increases oxygen levels in the home.
This short duration of open windows will not cause significant heat loss but will create a clean breathing space for your child’s airways throughout the day. This basic winter asthma cough prevention method requires little effort on your part.
2. Winter Bedding Protocol
The process of sun drying all blankets once per week even under cloudy weather conditions will eliminate mites through UV light exposure.
Switch your heavy wool blankets with layered cotton blankets which you can wash every month. Choose comforters that are designed for your local climate conditions and can be washed.
This step removes most hidden triggers from bedding which parents fail to recognize as asthma triggers during nighttime.
3. Air-Quality Routine for School Mornings
Your child can pre-warm their inhaled air through soft cotton coverage of their nose and mouth during commutes. Schools should avoid conducting PT classes during winter month mornings when outdoor pollution is at its peak.
Your child should learn nasal breathing because mouth breathing leads to lung exposure to cold air. These steps reduce morning airway spasms to a significant extent.
4. The “Two Room Rule”
Your child’s bedroom should be a completely separate space from kitchen fumes even though the kitchen door remains shut. The combination of winter indoor cooking near living spaces leads to extended particle suspension in air.
Your home should have designated sleeping areas which stay free from cooking smoke regardless of how well you ventilate other parts of your house.
5. Winter Nutrition Add-Ons
Your child’s diet needs the addition of foods that contain Vitamin D; egg yolks, fortified milk, and sun-exposed mushrooms serve as essential sources of this nutrient. Walnuts and flaxseeds contain omega-3 fatty acids which work to reduce airway inflammation.
Adding turmeric in milk and black pepper in meals will help you achieve warming effects. Replace cold water with warm ajwain or ginger infused water.
Our pediatricians employ nutritional therapy as a part of childhood asthma treatment plan because this approach helps to fight inflammation from within.
These preventive measures help you handle the seasonal asthma worsening by addressing winter-specific environmental and lifestyle elements directly.
When the Worsening Requires Medical Attention?

Home care should not be a substitute for professional medical assessment when children show these particular red flags. The following unusual warning signs need immediate medical evaluation:
- Your child develops fast breathing after waking up, suggesting their airways got inflamed while they slept.
- The child coughs only after experiencing hot-to-cold temperature changes which indicates hyperreactive airways.
- The child experiences wheezing at night even though the room stays warm which suggests other factors than temperature are causing the issue.
If you notice any combination of these patterns, consult Dr. Saba Ekta at Dr. A Barkat Multispeciality Hospital in Gaya.
The hospital offers specialized services including:
- NICU and PICU care
- Child Development & Growth monitoring
- Comprehensive diagnosis and treatment for childhood allergies
- Expert management of infectious diseases
- 24/7 emergency and medical care
- Comprehensive vaccination programs
Having the best child doctor in Gaya helps rule out hidden medical issues that need specific medical intervention. As the best emergency hospital in Gaya, our facility is equipped with emergency care capabilities for infants and adolescents. The evaluation process at the doctor’s office will help you understand what temperature is too cold for asthma for your child and what specific triggers affect them.
Protect Your Child’s Breathing This Winter
Winter asthma goes beyond your child’s exposure to cold temperatures, and it often stems from regular household habits, environmental factors, and lifestyle choices.
The winter season brings multiple triggers, and parents usually seal their homes, use thick bedding, and keep their children inside in a bid to protect them.
However, your child can achieve better respiratory health during winter through basic changes to ventilation systems, bedding protocols, and daily morning routines.
Our pediatric team at Dr. A Barkat Multispeciality Hospital will deliver personalized medical care through scheduled consultations which will address the unique requirements of your child.
The hospital’s detailed evaluation enables families to identify which winter triggers are manageable and which require medical help so they can avoid child asthma triggers throughout the winter months.
So, don’t wait for symptoms to escalate. Schedule a consultation at Dr. A Barkat Multispeciality Hospital for comprehensive pediatric care now.




Leave a Reply